
Rajit John Cherian, Melvin J George, Jerin Thomas, Mathew Abraham
Mosc Medical College, Kolenchery, Kerala.
*Corresponding Author: Rajit John Cherian, Mosc Medical College, Kolenchery, Kerala.
Received date: November 22, 2022
Accepted date: January 20, 2022
Published date: January 27, 2022
Citation: Rajit John Cherian, Melvin J George, Jerin Thomas, Mathew Abraham (2022). “Closed Isolated Lateral Talar Extrusion - A Case Report’’. J Orthopaedic Research and Surgery, 3(1); DOI: http;//doi.org/03.2022/1.1024.
Copyright: © 2022 Rajit John Cherian. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
,
Introduction
Of all the talar injuries, Total talar dislocation (Talar extrusion) is a rare injury. It usually follows a high energy trauma and is usually associated with wound, associated fractures, severe soft tissue insult and disruption of talar blood supply. It accounts to about 2% of all talar injuries. Extrusion without an associated fracture is extremely rare. It is a combined dislocation of tibio-talar, talo-calcaneal and talo-navicular joints and is also known as luxatio tali totalis [1,2].
Closed isolated lateral talar extrusion is not even reported before. Being a rare injury, no definite treatment guidelines exist in literature for this type of injuries. Some authors advocates re-implantation of extruded talus; however, tibia calcaneal fusion may be needed in the long run due to high incidence of avascular necrosis and osteoarthritis [3]. We report a case of Closed isolated lateral talar extrusion in a 22 year old male which was treated conservatively due to some other reasons.
Case Report
A 22 year old construction site male worker was brought to the Emergency Department with a history of RTA, twisted his right foot under the two wheeler and was unable to move his right foot. On examination, there was an undue prominence over the lateral aspect of his right ankle and the whole foot was inverted. Toe movements were normal and there were no neurovascular deficits.

Fig. No: 1 – The deformity of the foot at the time of presentation to Emergency Room

Fig. No: 2 – The prominence seen over the lateral aspect of the ankle
On radiographic examination, he was diagnosed to have complete talar lateral extrusion without any associated fractures.
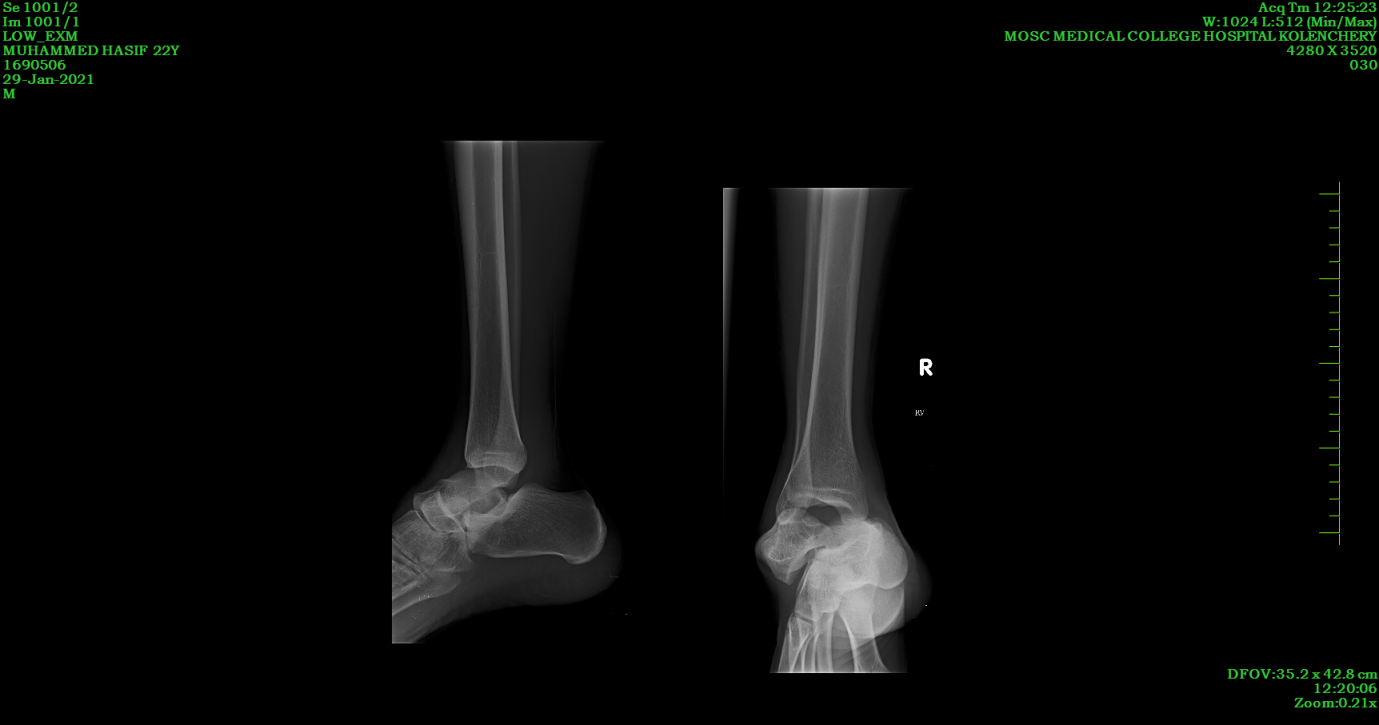
Fig. No: 3 – Radiograph demonstrating total lateral talar extrusion
The patient underwent closed manipulation and reduction in the emergency room itself under sedation. The need for closed reduction under anaesthesia was explained if manipulation failed. Foot was manoeuvred by traction over calcaneum, medial push onto the talus and then dorsiflexion. Repeat X ray revealed a reduced ankle and the joint was immobilised in a below knee POP slab.

Fig. No: 4 – Radiographic image after manipulation and reduction
Since such injuries are almost always associated with other fractures, Computerised Tomography was done to rule out any associated injuries.

Fig.No:5 – CT images of the ankle after Closed Manipulation and Reduction.
He was immobilised in a below knee slab for 2 weeks and when swelling subsided, converted to a cast for another 6 weeks. He was advised MR imaging for further evaluation, but denied due to financial constraints. Complications like avascular necrosis, secondary arthritis and stiffness were explained.
On review at 8 weeks after the injury, ankle was stable, with painful ROM at extremes. He was advised ROM exercises, ankle binder, weight bearing as tolerated with walker for the next 4 weeks.
At 3 months review, he had near - full range of movements, antalgic gait. At 6 months review, he has complete ROM, full weight bearing walking was painless and has resumed his work. At 1 year review his ankle was normal with no limitation in activities, and radiological evaluation showed no arthritis / AVN changes. Like before he denied further MR evaluation.

Fig. No: 5 – Clinical images at 1 year follow up.


Fig. No: 6 – X ray images at 1 year follow up.
Discussion
Talar dislocations are very rare. Most are Open dislocations resulting from high velocity Road Traffic Accidents and associated with extensive wounds or other fractures. Almost 54% of talar dislocations are open injuries. Complete dislocation without a concomitant fracture is extremely rare [4]. It was first reported by the German surgeon Fabricius Hildanus in 1680. The injury was treated by talectomy [5]. Complications associated with such injuries are re-dislocation, infection and avascular necrosis. The anatomy of the talus plays an important role in these complications. Talus doesn’t have any muscular origins or insertions and is covered by articular cartilage for upto 60% of the surface. Hence vascular penetration is restricted to a very small surface. The incidence of avascular necrosis depends on the integrity of these anastomoses and the surrounding soft tissue damage.
Total talar dislocation is thought to be the endpoint of maximum pronation or supination injuries. Leitner described a 3-stage mechanism of anterolateral dislocation with medial subtalar dislocation being the first stage [6]. The vascular anatomy of the talus has been well described by Gelberman and Mulfinger [7]. The talar body receives its blood supply from the tarsal canal artery, a branch of the posterior tibial artery, from deltoid branches of the posterior tibial artery and from the sinus tarsi artery formed by the anterior tibial artery and perforating peroneal artery. The talar head receives its blood supply from branches of the dorsalis pedis and from branches from the tarsal sinus artery. There is a network of intraosseous anastomoses, which are complete in approximately 60% of cases. The occurrence of avascular necrosis is determined by the importance of these anastomoses and the amount of soft tissue damage. If strands of the superior talonavicular ligament remain attached, avascular necrosis may be avoided [8].
Detenbeck and Kelly reported a very poor prognosis and believed that avascular necrosis almost always accompanies a total dislocation [9]. Infection developed even in closed injuries. However, Palomo-Traver, in a meta-analysis, reviewed all published cases until 1997 and after exclusion of the Detenbeck and Kelly series, he found a much better prognosis with no infections in closed injuries and 27.3% in open injuries, whereas the risk of avascular necrosis was 20% and 18.2% respectively [10].
Given the rarity of talar dislocations, there is no established treatment protocol. Some Authors recommend primary talectomy with tibiocalcaneal fusion, even in closed injuries [9]. Palomo-Traver suggested reduction except in cases with gross contamination or complete extrusion [10]. Closed or open reduction has been mentioned as the treatment method of choice [11,12 ]. Satisfying long-term results with good clinical outcome and no signs of avascular necrosis or arthritis have been reported [12]. If there is tendency to redislocation, K-wire trans-fixation may be performed. Most authors recommend an additional immobilization for six to eight weeks using a cast or external fixator [12].
In our case, reduction was done within 2 hours of the accident in the casualty itself, ankle was immobilised for a period of 2 months, good compliance of the patient with physiotherapy protocol; everything might have added to the happy ending of this story. But we cannot pass on the message of closed manipulation and reduction for such injuries due to the complexity of the injury and the instability element with just a Plaster of Paris supporting the reduction. This man has to be followed up long term for AVN and secondary arthritis.